FEATURE
A.I. and Health Care
Tools created by faculty, student researchers designed to help medical team improve care for patients with rare diseases

STORY BY MICHELE COFFILL / PHOTOS BY KENDRA STANLEY-MILLS
For people who have epilepsy, it’s often a trial and error process through several of the 30-some antiepileptic drugs to get to a medication that works.
Imagine, though, a situation where physicians and health care teams could explore a patient's dashboard — uploaded using artificial intelligence tools — and then prescribe personalized medication without trial and error. What if those same AI tools could help patients with rare diseases?
Zachary DeBruine, assistant professor of computing, and a team of student researchers are exploring how to develop and deliver artificial intelligence tools to help clinicians at Corewell Health and Helen DeVos Children's Hospital who treat patients with rare diseases.
Dr. Caleb Bupp, who leads Corewell Health's Medical Genetics and Genomics Division, said DeBruine's research could be invaluable in a medical field where 1 in 10 Americans has a rare disease yet 95% of patients have no treatment.
”We're cooking with gas now,” Bupp said.
Rare diseases have generally been studied individually
AI can provide insights into rare diseases collectively
Rare diseases have generally been studied individually
AI can provide insights into rare diseases collectively
DeBruine joined Grand Valley’s faculty in 2022, after working for nearly a decade at Van Andel Institute (VAI) as a post-doctoral fellow and adjunct faculty member. DeBruine’s work at VAI was groundbreaking in helping researchers store and analyze massive sets of biomedical data. It also provided a foundation for his work at Grand Valley centered around building generative AI tools for clinicians and researchers.
”We’re trying to develop genomic intelligence for clinical practice,” DeBruine said. ”This will put AI tools that understand not the English language like ChatGTP but the language of genetic regulation and genetic variation in the hands of clinicians so they can ask questions and get answers that help them improve patient care.”
Bupp said one of the many challenges of working with rare disease patients is the lack of comparisons to other patients. With DeBruine’s genomic intelligence tools, Bupp said he and his team are uncovering layers of understanding with patients.
For example, Bupp explained one ultra-rare condition that affects only 16 people worldwide. ”We can treat a few people by repurposing a drug we know works well. With Zach’s team, we're getting beyond the chemical reaction to the ’Why did this work?’” he said.
Bupp said genetics as a field used to be very reactive. With the advance of AI, ”We are shifting to being more proactive and Zach and his team are helping us to do that. They’re not giving us a road map but they're getting us in the driver's seat,” he said.
Zach DeBruine pictured
at the GVSU Reach Higher
Showcase in April.

The three organizational partners, Grand Valley, Corewell Health and VAI, have provided support and funding to create AI models that can provide collective insight into rare diseases.
Their first focus was pediatric epilepsy, a subject DeBruine understood well. His son, Andrew, was diagnosed with the disorder at birth. DeBruine explained to an audience during a Grand Rapids Tech Week event that Andrew underwent three different drug therapies, which is not uncommon for patients with epilepsy. Andrew is now 8 and healthy and happy, DeBruine said.
In the AI model DeBruine and his students are building, results from a simple blood draw would be uploaded to an app that generates an AI cell atlas that can be explored through a dashboard for physicians and clinicians to prescribe personalized medication to treat, for example, Andrew’s epilepsy.
”If we can learn a model that understands the language of genetics, that model would be applicable not only to pediatric epilepsy but also rare disease diagnosis,” DeBruine said.
DeBruine's approach to
personalizing health care
with generative AI:

DeBruine's approach
to personalizing
health care with
generative AI:

Zach DeBruine and students who work in his lab meet with President Philomena V. Mantella during Student Scholars Day.
Zach DeBruine and students who work in his lab meet with President Philomena V. Mantella, third from right, during Student Scholars Day.
Student researchers gain invaluable experience
Nine students work on this research in DeBruine’s lab, supported by a $200,000 grant from the Chan-Zuckerberg Institute. He also teaches an ”AI Innovation” class, and a smaller team of students presented its research on this topic at Grand Valley’s Reach Higher Showcase in April.
Skyler Ruiter worked in DeBruine's lab after learning of the opportunity through Grand Valley’s Applied Computing Institute. To say it worked out well for Ruiter would be an understatement.
Ruiter, who earned a bachelor’s degree in computer science in April, presented with DeBruine at the 2024 Data Compression Conference in Utah, where they touted the data compression library they created for public use. Ruiter is now in New Mexico as a summer intern for the U.S. Department of Energy’s Sandia National Laboratories.
Seth Wolfgang also earned a degree in computer science. As a member of DeBruine's lab, Wolfgang, from Zeeland, said their work was similar to building a high-performance computer.
”I spent hours every night to make sure I did this right,” Wolfgang said. ”You cannot have an AI model that is not working right.”
DeBruine said the opportunity to mentor and work with undergraduate students was partially what drew him to Grand Valley.
”In computer science, we tend to think more in the industry mindset. But it’s a goal of this project to bring academic challenges to the foreground to students who want to pursue a Ph.D. or go on to graduate school,” he said.
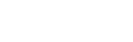
Connections to Blue Dot
Research from Zachary DeBruine, assistant professor of computing, and students in his lab is one example of the impact Blue Dot, Grand Valley’s initiative to support emerging technology and connect education with industry and business, will have in West Michigan and beyond.
DeBruine said the infrastructure of Blue Dot connects individual partners to solve problems for the greater good. In this case, DeBruine and his research team are developing tools using artificial intelligence to create a working AI model for medical teams to use to personalize medicine for patients with rare diseases.
Dr. Caleb Bupp, division chief, Medical Genetics and Genomics at Corewell Health and Helen DeVos Children's Hospital, said the leadership from top executives at Grand Valley and Corewell Health has opened the door to this partnership and more connections.
”This is among the priorities of President (Philomena) Mantella and Tina Freese Decker (president and CEO of Corewell Health),” Bupp said. ”Here we have two great leaders looking at their local organizations and seeing the connections. Grand Valley is driving toward AI innovation, so this is a natural partnership.”
Late last year, Gov. Gretchen Whitmer signed a $616 million supplemental funding bill during an event at Grand Valley, providing a $30 million boost to the university’s Blue Dot initiative.