Blog
Permanent link for Climb Every Mountain on March 31, 2021
Climbing workouts for better performance
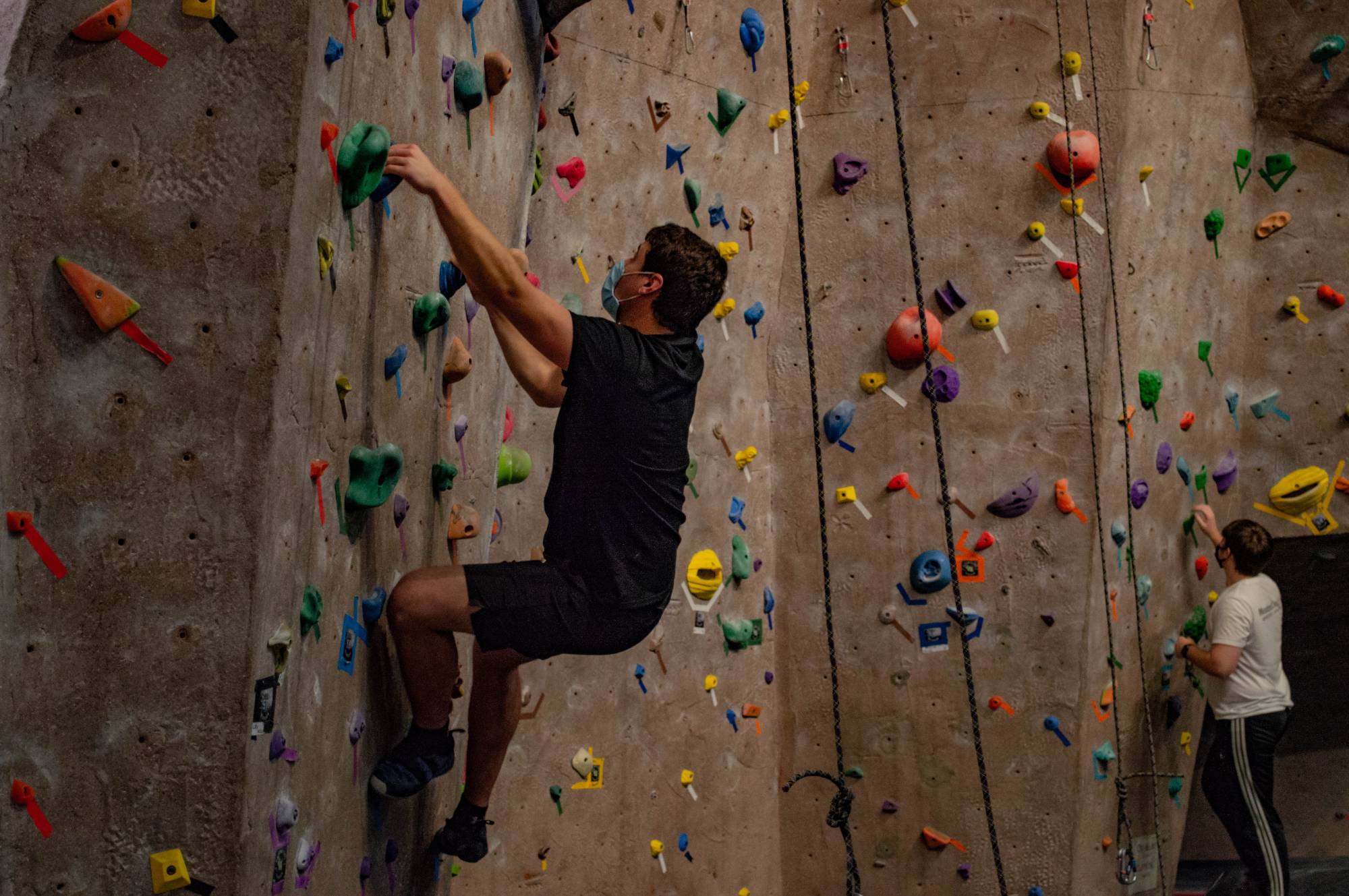
As with any sport or new hobby, there is a burning desire to push yourself to become the best you can be. As humans, we want to see how far we can go and how far we can push the limits of what we believe is possible. This may all seem very deep and philosophical, but if you take time to think about what drives you to be better, it will unlock new potential within yourself. For me, the pursuit of climbing hard grades and performance is what motivates me the most. But, the reason for training and climbing may be different for everyone. I encourage you to find the purpose of your training and remind yourself of this when you feel yourself falling into that inevitable rut. It is important to note that noticeable improvements don't happen overnight, and to our dismay, can take much longer than we would like. The ability to stay inspired and be encouraged is often what separates the good from the great. Not every workout or drill will work the same for everyone; one exercise might work for you but not for others. Trying each exercise and doing your own research through trial and error will help you dial in the workout routine that works the best for you.
CLIMB MORE!
The number one thing new climbers can do to get better is climb
more often! I can't stress this enough; climb more. It may seem
obvious, but getting in the climbing gym and on the wall is the best
way to build a solid foundation. Climbing two to three times each week
is a good balance for getting better each time you go to the gym,
without the added risk of injury you get from overtraining . A common
misconception is that strength is the magic key to unlocking new
routes. However, it's not always a lack of strength holding you back.
You might be able to do 50 pull ups in a row, but if you have no
technique, it will be hard to be a successful climber. It is true that
people with massive amounts of strength can likely climb hard grades,
but it often looks clunky and ends up wasting significantly more
energy than someone with good technique. Luckily, technique is one of
easiest and most enjoyable aspects to train. The number one way to
work your technique is to climb more, and with easy to do drills, it
can be fun.
TECHNIQUE
Climbing can be hard work but not every training session needs to
be physically exhausting for you to get better. Compared to strength
training, focusing on improving technique often results in bigger
improvements in a shorter amount of time. Especially for newer climbers.
Some drills for building technique:
Silent Feet: This drill is pretty simple and requires almost no gear. All you will need is a relatively easy section of wall. Then:
- Climb while making little to no noise when your feet touch the holds. This will require you to move slowly and with precision.
- Climbing with controlled motions requires you to find and remain in balanced positions.
- The goal is to improve your footwork, which is essential to be an efficient climber. In the long run, it will help preserve energy on the wall.
- Progress this exercise by applying it to specific paths, or “routes” on the wall and/ or adding bells to your shoes.
Single Touch: This drill works footwork, as well as precision with your hands. Pick a section of wall or two to three routes you can comfortably climb. Then:
- Once you grab a hold with your hands or place a foot on a hold, you can not move it unless moving to the next hold. You must hold the rock in the way you initially grabbed it, no shuffling around to find the best way to hold it. Repeat the same way for feet on foot chips.
- The goal is to increase precision with your hands and feet. Grabbing the hold exactly where you want to on the first attempt will save energy and help you from falling because of poor hand or foot placement.
There are other drills out there that improve technique, but these are the two that I personally use and have found success with. These drills work great as warms ups while improving the “smoothness” in your climbing.
ENDURANCE
The biggest downfall almost all climbers have is the fight
against the “pump” (or the build up of lactic acid in the forearms,
which signals fatigue of the fingers and arms). Stamina is essential
to climbing all types of routes and something I personally struggle
with the most. The ability to complete multiple hard moves in
succession is something that many climbers strive for. Training your
endurance is challenging and can be physically exhausting.
Fortunately, training for building climbing endurance is one of the
most fun types of training because it’s all about spending more time climbing!
Some drills for building your endurance:
Laps: This drill is very simple but is definitely taxing on the upper body. It is preferably done on a taller roped climb (aka a “top rope”) route but doing it lower to the ground, without ropes (aka “bouldering”) would suffice. The only downside of this drill on the top rope is the responsibility of the belayer (person controlling the rope and keeping the climber safe) to belay you multiple times in a row.
- Pick an easy section of wall or route that you believe you can comfortably climb twice in a row, but would struggle on your third attempt. Picking the right one is important; find a balance between pushing yourself but not going too hard. If you have a particular style you’d like to focus on, picking a route of that style would be a good idea.
- Simply climb the selected route three times in a row, only taking a break to chalk up and to check with your belay before climbing again.
Traverse: Similar to the laps drill, this will require you to be on the wall for an extended amount of time. This drill is more accessible, as it does not require someone to belay for you. The biggest downside of this drill is that if the wall is busy, you won't be able to do it.
- The goal is to travel across the wall horizontally for as long as possible. Or for a predetermined amount of time or moves.
- Climb below the boulder line on a side of the wall, then start climbing across the wall horizontally, using any hand holds you want and using foot holds smaller than a fist.
Hang boarding: This is a great way to strengthen your fingers from the comfort and convenience of your own home. As far as pure finger strength building goes, it's unbeatable. However, if you hang board too hard, too soon, or too often, they do present the risk of injury. I wouldn't recommend getting into hangboard training at all until you have climbed for about a year. Your fingers are the most important body part in climbing, so it's essential to keep them healthy. If hang boarding is something you are looking to get into, I encourage you to do some research beforehand. There are a lot of great, yet vastly different, workouts available. Hang board at your own risk!
Ringing the Bell
Rock climbing has endless possibilities. From the many gyms to
the thousands of established routes outside, there is something for
everyone to climb. With each harder grade you can climb a whole new
set of routes and areas open up for you to explore. For me training
has been a way to stay dedicated to the sport and stay in shape for my
own physical well-being. I learned the drills I discussed from those
who are more experienced than me, along with help from the internet.
Everyone has different ways to train so asking and discussing with
others is a great way to expand your knowledge and make a few new friends.
By: Owen Dingledine
Categories:
Outdoor Adventures
Posted
on
Permanent link for Climb Every Mountain on March 31, 2021.
Permanent link for What if we Daydream and Play instead of Hustle and Grind? on March 30, 2021
Many of us find ourselves in a revolving door of hustle and grind. School, work, life, repeat. There’s often little priority given to resting because rest can be seen as lazy and unproductive. But, research suggests that isn’t true. Just look to nature – even the trees and the plants and the soil and the animals take breaks to be the best that they can be. Yet, in the middle of an on-going pandemic, we continue to grind – but as the great Nap Bishop Tricia Hersey says – “You are not a machine. Stop grinding.”
What if instead we dilly-dally, daydream, rest, and play more?
Why the Grind Needs to Stop
Well, simply: We. Are. Burnt. Out.
85% of college students report being overwhelmed by everything they had to do at some point within the past year. 1 in 3 working adults feel burnout in the workplace. And for what? We lose $500 billion each year in lost productivity and 550 million working days due to stress on the job. It’s such a problem that the World Health Organization officially included burnout in its International Classification of Disease.
Our productivity doesn’t go up when we grind either. In fact - we are more productive when we rest. When we give ourselves a chance to slow down and take a break, our brains are sharper, we’re more creative, get more done in less time, make better decisions, prevent illness, and are able to review and reflect on our days. And, even if our productivity did go up when we were grinding - our pay hasn’t gone up, so why are we doing it if we haven't seen a return on investment?
How to Stop Grinding: Finding Balance to Avoid Burnout
One of the best ways we’ve found to avoid burnout and find
balance in life? Set boundaries - with your friends, family and
yourself. It can be hard, but with practice you will make time to:
engage in self-care, find enjoyment, spend time on hobbies, connect
with friends, get some exercise, sleep a little (or a lot) and so much more.
So, how do you set boundaries? Here are few tips:
- Seek help . Reach out to those that can help, including professors. They can give you tips for succeeding in their courses.
- Conduct a personal audit of situations, times, or people that cause you stress or anger. This helps you recognize these circumstances in the future so you can be prepared and have strategies already in place to help you cope.
- Choose and set clear limits for yourself. Many times the people that cross our boundaries the most are us. It’s vital that you determine what goals or activities are most important to you (like rest, exercise, family, cooking meals, getting good grades, etc) and keep them at the top of your priority list.
- You should communicate your boundaries with those around you, particularly those that are most likely to cross them. And, it’s important to let someone know when they’ve crossed one of your boundaries when they do it.
- Practice saying “no.” No’s tend to be super hard for people to say. So it’s important to practice saying no in low risk situations - like getting a coffee for example. When they ask if you want whipped cream with that…. no. Practice in front of the mirror - wherever, whenever so when you really want or need to say no you can.
- Use the 4 D system. When you make a to do list, determine if you are going to do it now, defer it to another time, delegate it to someone else (like if it’s a group project or if you’re in a student organization, etc), or drop it - and just decide it’s something you don’t have to do at all.
- Finally, prepare for pushback . People don’t often get told no or have people enforce boundaries (because we’re pretty bad at doing it as a society). So, know that others will likely react to you enforcing boundaries - this just means the boundaries were necessary. (Also, don’t forget, you are most likely to step over your own boundaries so be prepared to keep setting boundaries for yourself!)
Keep Pressing Pause
Our societal culture of hustle and grind is why Recreation &
Wellness created the Press
Pause campaign for Winter 2021 – a gentle reminder to give
yourself a break. Remember, that it’s okay (and vital) to rest. Even a
five minute pause in our days can lower our heart rate, loosen our
muscles, increase immunity, improve sleep and digestion, and elevate
our overall well-being. The semester is coming to an end and we know
that stress and burnout will be even more pronounced. So, plan time to
press pause and honor your boundaries. And - don’t forget to keep
pressing pause into the spring and summer.
Wishing you a day (month, year, life) full of daydreaming, dilly-dallying, resting, playing, and contentment.
Want to learn even more? Request a WIT presentation about Finding Rest in the Grind.
By: Katie Jourdan, Student Health Promotions Coordinato
Categories:
Rest
Posted
on
Permanent link for What if we Daydream and Play instead of Hustle and Grind? on March 30, 2021.
Permanent link for Sexually Transmitted Infections on March 29, 2021
Part of our Sex-Ed Series
April is STD Awareness Month so we’re getting a head start and taking some time to share about STDs (though we’ll call them STIs throughout the blog because that’s the newest, most accurate description).
Sexually transmitted infections (STIs), previously known as sexually transmitted diseases (STDs) or venereal diseases (VD) are infections that are passed on from one person to another through sexual contact. This contact is usually oral, vaginal and/or anal sexual activity. However, sometimes STI can also spread through other intimate physical contact, like herpes, human papillomavirus (HPV) which can spread through skin to skin contact as well. STI can spread through five fluids; namely, vaginal fluid, semen, breast milk, blood and rectal fluid. They spread through genital skin-to-skin contact, genital-to-mouth, genital-to-anus, mouth-to-anus, anything-to-sex toy and sharing things during a sexual activity.
If not diagnosed early or left untreated, STIs can cause serious health-complications, including, but not limited to Pelvic Inflammatory Diseases (PID), infertility, mother-to-child transmission (example HIV, neonatal-syphilis) and neurological manifestations.
The most common symptom of an STI is: no symptom at all. Other common symptoms present are unusual looking/smelling discharge, itching or burning sensation in the genitals, or pain during sexual-intercourse.
What does our data say about STI prevalence?
According to CDC’s
Survey of 2018, one in five individuals in the
United States has an existing STI. In 2018 alone, there were 26
million new cases of individuals who tested positive for an STI in
the United States, and half of them were 15-24 years old.
They are prevalent among individuals irrespective of their
gender or sexual-orientation.
Exploring Some Sexually Transmitted Infections
We’ll share just a little about each infection below, but learn
more comprehensive information about each through the CDC.
Viral Infections: Viral infections are caused by viruses. They are treatable but cannot be cured.
- Human ImmunoDeficiency Virus (HIV) infection weakens a person’s immune system by destroying important cells that fight disease and infection. In its advanced stage or when left untreated it causes Acquired Immunodeficiency Syndrome (AIDS), which results in failure of the immune system and can be fatal. AIDS is Stage 3 of HIV infection in which the number of T-cells present in our body decreases drastically compared to the normal count. However, most people in the U.S. do not develop AIDS anymore, and remain with a case of HIV, thanks to treatment options like antiretroviral therapy. Treatment options are so good now that a person can have undetectable amounts of HIV in their body and no longer transmit the virus. Legally if you have HIV/AIDS, you must disclose your positive status to all sexual partners before you have sex (any act that could spread the disease) and it is illegal to disclose anyone else’s HIV/AIDS status (positive or otherwise).
- Herpes - This common infection causes recurrent outbreaks of painful blisters (though most people don’t know they have it and may not have symptoms). There are 2 types of herpes viruses. The Herpes Simplex Virus-1 is oral herpes and Herpes Simplex Virus Type 2 causes genital herpes. Most people get infected with HSV-1, and it results in cold sores around the mouth. If this occurs, refrain from oral sex. HSV-2 results in blisters or sores around the genitals or rectum.
- Human Papillomavirus (HPV) - HPV is a common virus that can lead to certain types of cancer later in life. We have vaccination for HPV/genital warts and a vaccine for this STI is given around 11/12-years-of-age in all genders. Men are less likely to show symptoms but they can still pass it on to their partner(s).
- Hepatitis B - Hepatitis B is a vaccine-preventable liver infection caused by the hepatitis B virus (HBV).We have a vaccine for Hepatitis B STI at birth. Hepatitis B can actually be cured by prescription if treated immediately after exposure.
Bacterial Infections: Bacterial infections are caused by bacteria. They can be cured with antibiotic prescriptions. This is why it’s important to get tested and if you have an STI, to get treatment from your healthcare provider.
- Gonorrhea: A very common infection that can cause serious complications when not treated. Untreated gonorrhea may also increase your chances of getting or giving HIV – the virus that causes AIDS.
- Chlamydia: A common STI that can infect both men and women. It can cause serious, permanent damage to a woman’s reproductive system. It is often known as the “silent infection” because most people do not have symptoms.
- Syphilis : The infection is divided into stages (primary, secondary, latent, and tertiary). There are different signs and symptoms associated with each stage. If left untreated causes extensive damage to the nervous system.
Parasitic infections: Parasitic infections are caused by parasites or mites. They are curable by prescriptions and over-the-counter medications.
- Trichomoniasis: Is caused by infection with a protozoan parasite and usually has no symptoms. It is curable by prescription medicine.
- Pubic Lice (crabs) : Pubic lice typically are found attached to hair in the pubic area but sometimes are found on coarse hair elsewhere on the body (for example, eyebrows, eyelashes, beard, mustache, chest, armpits, etc.). Lise cause itching usually beginning after 5 days after contact, but they have no long term health effects. It is curable by over-the-counter medication or prescription.
- Scabies: The microscopic scabies mite burrows into the upper layer of the skin where it lives and lays its eggs. The most common symptom is itching. It is curable by over-the-counter medication.
How to Prevent STIs
The good thing about STIs is that they are preventable, getting
tested is no big deal, and most STI are easy to
treat.STIs can prevented by:
- Using barrier methods during sexual-activities can prevent STIs. These include internal and external condoms and dental dams. GVSU Recreation & Wellness partners with the Ottawa County Department of Public Health to provide external condoms through Wear One. Condoms can be found in several offices all around campus for students to pick up - for free.
- Participate in regular STI screening and health check-ups when you are sexually active.
Not sure about which test you need, the CDC has some guidance.
- Vaccination is another way to prevent some STIs. Vaccinating for Hepatitis B and HPV have medically proven to prevent the respective infections.
As they say, an ounce prevention is worth a pound of cure, it is equally true and applicable for Sexually Transmitted Infections and hence: Take control, be aware and educate yourself about STI and participate in safe sex practices.
By: Sonal Subhash Mandale, WIT Peer Educator
Categories:
Sexual Health
Posted
on
Permanent link for Sexually Transmitted Infections on March 29, 2021.
Permanent link for Covid-19 and Victim Survivors on March 22, 2021
Part of our Sex-Ed Series
We’re excited to welcome guest blogger, Ariana Deherder, Violence Prevention Student Assistant with the Center for Women and Gender Equity .
As we’ve reached the one-year mark of COVID-19 in Michigan, it is important to take a moment to reflect on how we are all experiencing collective trauma and grief. This pandemic has impacted everyone in some way, whether big or small. Those who are dealing with the stress and trauma from COVID-19 after already having suffered from sexual or relationship violence are some of those individuals being impacted in a big way. Victim survivors are uniquely experiencing this pandemic and can be affected differently than others. Although it may not be clear at first how there is a connection between COVID-19 and sexual violence, the following sections will help to explain this strong and harmful connection.
Domestic Violence
When thinking about COVID-19 and victim survivors, the first
thought that likely comes to mind is how those who are currently
living with an abuser are being harmed by stay at home orders. It’s
true that staying at home can be very unsafe for those living in
violent situations. This can increase their risk for domestic and
sexual violence, while simultaneously restricting access to outside
resources and supports, like friends and family. Abusers take
advantage of the pandemic by using it as an excuse to limit visitors
and deliveries, errands, canceling appointments, not allowing
survivors to work outside the home, and more. Given the context of the
pandemic and orders to stay at home and socially distance, this can be
interpreted as perfectly reasonable and can be much more difficult to
resist by the victim survivor. These are typical victim-isolation
tactics, but are now able to be excused as compliance with public
health guidelines. Additionally, many people are feeling the economic
burden of COVID-19. While this is harmful to anyone who is
experiencing it, those in abusive situations may be suffering unique
consequences. A loss of income could force victim survivors to stay
with their abusers. Although they could have been saving up money for
an exit strategy, they may have to now abandon this strategy due to
loss of income.
COVID-19 Retriggering Trauma
Victim survivors do not have to be currently experiencing sexual
or relationship violence to still be facing challenges and a
retriggering of their trauma during this time. Although the
conversation about COVID-19 and victim survivors typically stops at a
discussion about domestic violence, there is much more to unpack.Those
who have experienced sexual violence in the past are facing a
retriggering of trauma during the pandemic. Triggers
are defined as “memories stored in our physical and emotional selves”.
Those memories can resurface when experiencing specific sounds,
tastes, feelings, or events. Staying
at home may be triggering for victim survivors who were
assaulted in their homes, leading to anxiety, fear, or symptoms of
PTSD. Even if home is considered a safe space, having to remain at
home for prolonged periods of time can still bring up its own set of
challenges as the mere isolation of being at home can be triggering. A
feeling of isolation can be a long-term effect on victim survivors,
and that feeling is being heightened during the pandemic. Coping
mechanisms that victim survivors used previously to manage their
triggers, such as connecting with others, may no longer be as
effective given the current state of the world. Further,
many of us are currently experiencing changes in our body’s
systems. It is normal for people to be experiencing sleeping and
eating changes, high levels of anxious energy coupled with total
exhaustion, and more frequent dreaming and nightmares. While this may
be the first time some people are experiencing this at such a
heightened level, for victim survivors, this can be reminiscent of
what their bodies and minds endured in the early stages of recovering
from sexual violence.
Medical care for victim survivors
Medical care for victim survivors are being impacted by the
COVID-19 crisis as well. Forensic exams are
examinations provided to sexual assault victim survivors to gather
evidene that is suitable for use in court. These exams typically need
to be conducted within 72 hours of the assault, as physical evidence
is typically gone after this time period. 85%
of forensic nursing programs in the United States operate out of
emergency departments, according to the International Association of
Forensic Nurses (IAFN). These emergency departments have noticed a
significant decrease in the volume of patients seeking non-COVID
related care. The IAFN conducted a survey that found that 4 out of 5
programs have noticed a decrease in the number of patients coming in,
with almost all of them describing it as a “noticeable decrease”. This
could largely be a result of victim survivors fearing infection if
they enter an emergency department or hospital. Under normal
circumstances, forensic exams can take 4 hours or longer to complete,
so it is not surprising that a victim survivor may feel hesitant to be
in a hospital for that long. They may also be impacted by the social
messaging we are experiencing right now that encourages people to make
sacrifices for the greater good, such as avoiding entering hospitals
and burdening an already overwhelmed healthcare system. Even if a
victim survivor does decide to enter a hospital, the
experience is changed. For a while during the pandemic, trained
victim advocates were not allowed to accompany the victim survivor to
the exam, leaving them alone during possibly one of the most traumatic
times in their lives.
Coping Skills
As mentioned previously, prior coping skills that a victim
survivor might have engaged previously may no longer be as effective.
It is important to develop new coping skills and new routines given
the circumstances of the pandemic. Here are some ideas:
Body Calm
- The first part of recovering after a traumatic event is to calm
the body and the activation of the nervous system. To accomplish
this, try some of the following techniques:
- Breathe mindfully: place one hand on your chest and one on your stomach, and do 4 second inhales, a 4 second pause, and then a 4 second exhale. Set a timer for a minute or two and do nothing but mindfully breathe
- Low intensity exercise: high intensity workouts can exacerbate your nervous system while it is working hard to regulate itself. Therefore, workouts like yoga, swimming, pilates, or walking that won’t raise your heart rate too high are a great option for bringing your body some calm. Bonus points if you can be outside while doing this!
- Make sure you’ve eaten: It can be easy to forget to check in with your physical needs, so take a minute to check in with your body and assess whether you’ve eaten enough or drank enough water.
- Trauma informed yoga: This can be a great way to bring your body some calm without raising your heart rate. If you are interested, check out the trauma informed yoga CWGE is putting on in collaboration with RecWell for Sexual Assault Awareness Month!
Mind Calm
- After calming down your body, victim survivors may still
experience racing thoughts or triggers. Here are some suggestions
for how to bring your mind some relief after you’ve done so for your
body:
- Journal: in documenting your thoughts, you may want to acknowledge that you are reliving memories of the trauma. Try asking “when did I know I was safe after that happened?” Gently move your thoughts to when you knew you were safe, rather than the traumatic event itself. Continue asking yourself what or who has made you feel safe since then? Let the prompt take you where you need to go
- Reach out to a safe person: reach out to someone who you feel safe with and supported by. Send a text, have a video chat, phone call, or socially distanced meet up.
- Watch a comforting show: Watching a show, especially one you’ve seen before, can bring a sense of comfort and predictability to a time that feels very unstable and unpredictable. Cuddle up with a blanket, a furry friend if you have one, and indulge in some Netflix!
- Say affirmations aloud: affirmations can be a powerful and grounding tool for when you are struggling. Cassandra Corrado has some wonderful affirmations specifically tailored to victim survivors on their website.
If you are interested in hearing more about this topic and diving deeper into the connection between COVID-19 and victim survivors, join the Center for Women and Gender Equity on April 7th at 4:00pm. Register for the event using the following link. Check out the Center for Women and Gender Equity’s other events for Sexual Assault Awareness Month as well. See you there!
Take care of yourself, Lakers!
By: Ariana Deherder, Violence Prevention Student Assistant
Categories:
Sexual Health
Posted
on
Permanent link for Covid-19 and Victim Survivors on March 22, 2021.
Permanent link for The Racial Sleep Gap on March 18, 2021
I can never sleep before the first day of school. The night before my first day of 6th grade, I remember tossing and turning; the nerves and stress about the day ahead take over any exhaustion in my body. This happens to me every year and most of us have been there. But for many, it's not just the night before the first day of school or a big test, it's every night.
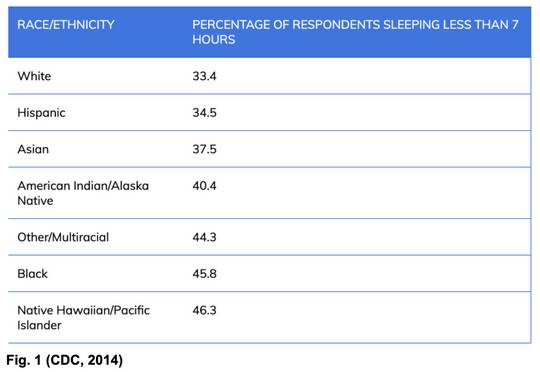
People of color are less likely to get 7 or more hours of sleep due to several racist factors. This creates a gap, or inequality, in sleep. Sometimes, in order to truly see the seriousness of this issue, it helps to see a visual (see Fig. 1). The CDC conducted a survey where they asked 444,306 American adults about their sleep patterns. The results are alarming; 34.5-46% of non- white adults were getting less than 7 hours of sleep per night with higher percentages of those that identify as Black or Native Hawaiian/Pacific Islander.
Race and Sleep: The Facts
To put it plainly, white people tend to get more (and better)
sleep than people of color. The gap is increased even further between
the wealthy and the poor. This gap is due to race, income, and status.
These factors intersect
easily and cause an enormous amount of stress, which ultimately
affects sleep, health, and overall well-being.
Place of residence, work schedule, and job strain, amongst other factors, play the biggest roles in the racial sleep gap.
- Place of Residence: In a study of around 33,000 participants, researchers found a direct correlation between sleep loss of African American and Hispanic people who live in inner-city areas compared to people who live in non-urban areas.
- Work strain: Due to discrimination in the workplacework place, African American and Latinx Americans are more likely to work unconventional hours and are about three times more likely to experience job related stress. Non-white people have to work harder, smarter, and faster to get to the same point as a white person. This is an exhausting, everyday battle that decreases healthy sleep patterns and not only increases the sleep gap, but contributes to many other health issues.
- Financial stress: People of color are less likely to be considered for higher level jobs due to discrimination in the workplace, which keeps them in lower income brackets. When most of the monthly income is spent on food, shelter, and water, other necessities get put on the back burner For example, healthy, organic foods tend to be more expensive or not available in certain areas. If a person has a low income and/or lives somewhere with less access to nutritious foods, it is much harder to find wholesome options. This can cause increased health problems including obesity, diabetes, and heart disease. Additionally, working two jobs may be a necessity for those in lower income brackets, leading to working more hours, increased stress, and inevitably less sleep
- Unequal Access to and Quality of Medical Care: Disparities in access to care have a broad effect on health outcomes for minority groups. For example, conditions like sleep apnea may be less likely to be diagnosed or effectively treated, or people may be less likely to discuss sleeping problems with a doctor.
Why is Sleep Important?
Sleep is important because it allows the body and mind to repair
and prepare for another day. Sleep allows the brain to function
correctly, helps the body fight diseases, and is an important part of
keeping your heart healthy.
There is a direct link between long-term sleep deprivation and health problems. As fellow WIT peer educator, Stella, notes in her recent blog post, “a poor sleep schedule can have very real, negative effects on people. Physically, you are at risk of a weakened immunity, weight gain, and heart-related problems such as high blood pressure and stroke. Maybe not so obvious, poor sleep is strongly linked to many mental disorders. It can impair your abilities to make decisions, cope with stress or change, and control emotions. These effects wreaked havoc on my life, and I didn’t even realize it was happening for so long!”
Lack of sleep targets your central nervous system, immune system, respiratory system, digestive system, cardiovascular system, and endocrine (hormone) system. When these body systems are out of tune, many serious health problems can occur, including:
- Memory and concentration issues
- Mood changes
- Weakened immune system
- High blood pressure
- Diabetes
- Obesity
- Low sex drive
- Heart disease
People of color experience these health problems at higher rates already, and they tend to experience even less sleep because of these health issues.
Wake Up and Smell The Racism
Sleep is so important. It re-charges us, mends us, and gives us a
much needed break from the craziness in our lives. While all humans
deserve a good night's sleep, not everyone gets the chance with the
inequalities that exist. The racial
sleep gap is a public health issue, and the United States needs
to do more to close it.
Understanding individual privilege and educating yourself on inequality, in all areas, is the first step. If you have the privilege of sleeping well each night, you can use your waking hours to raise awareness for sleep inequality. But how can you do this? By having impactful conversations with others who may not know or understand what the sleep gap is, supporting businesses owned and products made by people of color, and/or doing more research on inequality in America. Next time your head hits the pillow, you may think about things much differently.
By: Annie Seeber, WIT Peer Educator
Categories:
Sleep
Posted
on
Permanent link for The Racial Sleep Gap on March 18, 2021.
Permanent link for Sex While Menstruating on March 15, 2021
Part of our Sex-Ed Series
Can I have sex on my period? It’s a question that many people with vaginas have every month, and the answer is yes, you can! For the majority of people, having sex on your period is perfectly normal and healthy. It may seem “dirty” or dangerous to some, because period sex has been viewed as taboo for centuries. But, if you are comfortable, period sex can be mentally and physically beneficial.
Benefits of Period Sex
There are actually more added advantages of having sex while
menstruating than you might think. If you’re willing to deal with the
mess, you might experience some, or all, of the following benefits:
- Period cramp relief: menstrual cramps result from contractions of the uterus, and after an orgasm, those muscles relax to relieve the pain.
- Headache and migraine relief: during an orgasm, feel-good chemicals called endorphins rush through your brain, reducing your perception of pain. One orgasm could provide faster relief than an IV of morphine!
- Natural lube: the blood from your menstrual cycle can act as a natural lubricant during vaginal intercourse.
- Shorter periods: the intense uterine contraction that happens during an orgasm actually pushes out the uterine contents, possibly resulting in a shorter period.
- Increased sex drive: due to fluctuating hormones, your libido and desire can increase dramatically with the increase of estrogen in your system.
In the mood, but worried about the mess?
When it comes to period sex, there’s not really any way to keep
things totally clean. To make cleaning up as easy as possible, have
plenty of tissues and towels on hand. Things are going to get messy,
so try placing a towel underneath you and your partner to save your
sheets and mattress. Tissues are also nice to help with cleaning up
after the deed is done. Also, you could try having sex on a “lighter”
day of your period to reduce the mess.
Here are some other tips to help you have better period sex:
- Communication is key! Having an open and clear communication with your partner(s) regarding what you are comfortable doing is really important. Everyone should be on board.
- For anyone who has tested positive for HIV, hepatitis, or any other sexually transmitted infection, the likelihood of transmitting a bloodborne illness may be increased due to the presence of period blood. Using a barrier method of contraception is an effective way to prevent the spread of any STI.
- While it is less likely, getting pregnant is still a possibility during your period. As always, if you are trying to prevent pregnancy, barrier methods and birth control are suggested.
- If you use tampons or menstrual cups during your periods, it is strongly advised that you remove them before penetrative sex to prevent any injury or displacement of the items in the vagina.
For some people, having sex on your period can be such a liberating experience and a way to express your own body positivity in a fun way with your partner(s). But sometimes, you don’t want to deal with a mess, or maybe you are simply uncomfortable with it. No matter the reason, not wanting to have period sex is totally valid as well. Period sex can be a fun way to make the most of your time of the month in the bedroom, so don’t be afraid to embrace your sexuality and add some spice to your sex life!
By: Camryn Lane and Sonal Subhash Mandale, WIT Peer Educators
Categories:
Sexual Health
Posted
on
Permanent link for Sex While Menstruating on March 15, 2021.
Permanent link for The Wondrous World of Birth Control on March 7, 2021
Part of our Sex-Ed Series
Implants and patches and pills, OH MY! Oh, the wondrous world of birth control. With all the misconceptions, expectations, and varieties, getting the DL on birth control can be difficult on your own. Sadly, you can’t click your heels three times and magically have the perfect birth control method appear- trust me I’ve tried. But, with a little research, an idea of what you want, and an important chat with a healthcare provider, navigating the yellow brick road of birth control can be easy!
Types of Birth Control Methods
Birth control is any method, medicine or device, used to prevent
pregnancy, regulate the menstrual cycle, and balance hormones. Birth
control methods vary greatly, including 12
different types in total. With so much variety, there is a type
for every person and every lifestyle. In this blog, we will go over
the most common types of birth control. Whether you’re seriously
looking into birth control or are just curious, this post is for you.
The Pill
- Perfect use: 99% effective
- Typical use: 91% effective
Oral birth control, or the pill, is a contraceptive pill that contains hormones that stop ovulation. Since the hormones stop the ovulation, there is no egg for the sperm to fertilize. There are many different brands of birth control, each one affecting the body a bit differently. In order to do its job successfully, the pill is prescribed to be taken once a day. This can be a pretty big lifestyle change for some people, but there are tips and tricks to help you remember to take your pill: Download a birth control reminder app/set an alarm on your phone, keep your BC pills in a place you see them often (like next to your toothbrush, keys, or in your bag/backpack), or ask friends/partners/family to help keep you on track with taking your pill. Keeping an open conversation with your healthcare provider will make sure your birth control needs are being met.
The Implant
- Perfect and typical use: 99% effective
The implant is a rod inserted into the upper arm (by a healthcare provider) to prevent pregnancy. The rod releases progestin, which is a hormone that stops the ovaries from releasing eggs. The most common side effect of the implant is irregular bleeding, especially during the first 6-12 months after the implant is inserted. This form of birth control lasts up to four years, which is super convenient and perfect for someone with a busier lifestyle!
The Patch
- Perfect use: 99.7% effective
- Typical use: 93% effective
The Patch is basically what it sounds like, a patch, similar to a bandaid or sticker material. The patch has hormones on it that enter the bloodstream from the skin. Similarly to the implant and pill, the hormones in the patch stop the ovaries from releasing the egg, as well as strengthen the cervical mucus (which helps block sperm even more). It is important to note that there is a higher likelihood of blood clots while using the patch, so make sure to consider this when talking with a healthcare provider. The patch is applied weekly to the skin anywhere you want, except for the breasts. Similarly to the pill, you wear the patch for 3 weeks on, 1 week off “your period.” (Read more about how withdrawal bleeding on hormonal birth control is different than on a regular menstrual period.) You can also wear the patch four weeks a month, which skips your “period” for that month. Before doing this, make sure you talk to a healthcare provider.
The IUD
- Perfect use: 99.4-99.9% effective
- Typical use: 99.2-99.9% effective
An IUD is a little T shaped device, about the size of a quarter, that is inserted into the uterus (by a healthcare provider). The IUD is available in two different forms: hormonal and non-hormonal. The hormonal IUD keeps the ovaries from releasing the egg, while the non-hormonal IUD (made of copper) changes the way sperm cells swim, so they cannot reach the egg; sperm and copper do not like each other! The hormonal IUD commonly treats severe cramps during your period and lightens your period significantly, which is always a plus! Depending on your choice of IUD, it can last from 3-10 years.
The Vaginal Ring
- Perfect use: 99.7% effective
- Typical use: 93% effective
The vaginal ring is a malleable, latex free, plastic ring that is inserted into the vagina once a month for 3 weeks at a time. The ring contains the hormones estrogen and progesterone that keep the ovaries from releasing the egg. Similarly to other hormonal methods, it also thickens the cervical mucus to further protect the uterus from sperm. The vaginal ring also can ease menstrual cramps and lighten your period. Since the vaginal ring has less hormones than other hormonal options (like the pill and patch), side effects tend to be lower.
The Shot
- Perfect use: 99.8% effective
- Typical use: 96% effective
The birth control shot is basically an injection of the hormone progestin by a doctor or healthcare professional. It can be given in the arm or the hip, whatever is more comfortable for you. The hormones in the shot keep the ovaries from releasing the egg, but also have positive impacts on the menstrual cycle. The shot can help lessen cramps and lead to lighter periods.
Condoms
- Perfect use: 98% effective
- Typical use: 87% effective
Condoms (external and internal) are the only form of birth control that can prevent STDs! Which is VERY important! For all things condoms, visit our Sex Ed Series post on them!
Withdrawal
- Perfect use: 96% effective
- Typical use: 80% effective
The withdrawal or “pull out” method is basically how it sounds; the person with the penis pulls out of the vagina before they ejaculate. This is the oldest trick in the book. It’s free, but it's not the most effective when it comes to preventing pregnancy. (This method does not prevent STDs, so getting tested regularly is important.) You or your partner(s) would have to be a pulling out pro, since this method involves total body awareness, which can be pretty hard to accomplish.
Emergency Contraception
- Perfect use: 85% effective
- Typical use: 75% effective
An emergency contraceptive is a form of birth control used after unprotected sex. This form of BC is commonly found in an oral pill, well known as “the morning after pill.” It can be taken up to 120 hours (5 days) after unprotected sex, but this form of contraceotive works best the sooner you take it. It is important to note, if you weigh more than 195 pounds, the pill may not work as well. It is great to have this option as an emergency, but using birth control before engaging in sex (like an oral birth control) or during sexual activity (by using condoms) is the best way to prevent pregnancy.
How to Find What’s Best For You
Before you take the BC journey, it is important to ask yourself a
few questions. Knowing yourself, your lifestyle, and your BC goals
will guide you when searching for the best birth control method. If
you can, grab a pen/pencil and paper!
- What is your lifestyle? Do you have time for an everyday form of birth control? Would a less frequent method be best for you? Grab a pen and paper and write down your everyday schedule. What birth control method fits it best?
- What are you looking for? Pregnancy prevention, less painful period cramps, hormonal balance, lighter menstrual flow, reduced acne, non-hormonal method? Write which ones you are looking for down.
- Does your birth control choice affect your partner(s)? It can. It is important to keep an open communication with your partner(s) if you are planning on adding birth control or changing yours up. Many people have latex allergies, reactions to hormones like estrogen and progestin, or ingredients like dyes inside oral contraceptives. Remember, it is your body! Do what is best for you, but if your birth control needs include a partner, make sure to talk with them!
- Blood clots are more common (particularly for those over 35, or people who smoke) when taking birth control, due to the higher level of estrogen in hormonal contraceptives. It is very important to acknowledge this when deciding on a method. Do you smoke? Are you over 35 years old? Do you have a family history of blood clots? If you can, talk to family and/or do some quick research on clotting. Make sure you write down any questions or concerns you can bring up to a healthcare professional.
- For more info about birth control effects on cisgender and trans men take a look at this article.
Now, you've got all your birth control goals! This piece of paper is a great way to open communication with your doctor/healthcare provider if you don’t know where to start, since all your wants, needs, questions, and concerns are written down.
Next Steps
Now it is time to talk to a healthcare provider. This can be
pretty daunting; we aren’t in Kansas anymore… But do not fret!
Healthcare professionals are here to support you and should have your
best interest. When you go in for a birth control consultation, make
sure to voice your birth control goals: wants, needs, questions, and
concerns. From there, you and the healthcare provider will work
together to get you the best birth control for you.
Now, how do you pay for birth control? With the Affordable Care Act (ACA), most health insurance companies have been required to cover birth control at no copay in their plans. If you are on your parent’s insurance, you can call the insurance company and ask them about what happens after you make an appointment (ie. do they send an explanation of benefits that will show the service?). You can also ask your healthcare provider about billing for health insurance. They have lots of experience with this exact thing! You can also choose to not use your health insurance, it will likely cost between $15 and $50 a month.
Birth Control Break-Down
Whew! The wondrous world of birth control can be a lot.
Thankfully, by breaking it down, finding your birth control goals, and
having open conversations with your partner(s) and healthcare
providers, it can be much more simple. In any journey, there will
always be bumps in the road. Whether it was flying monkeys, giant
ditches, a roaring river, or a deadly poppy field, Dorothy had her
friends to get her through it. The GVSU Wellness Information Team
(WIT) is here for you too! We are not known for our poppy field
maintenance or flying monkey wrangling, but if you have any questions,
comments, or concerns please reach out to us using Ask WIT. For common
questions on birth control, visit our website.
By: Annie Seeber, WIT Peer Educator
Categories:
Sexual Health
Posted
on
Permanent link for The Wondrous World of Birth Control on March 7, 2021.
Permanent link for Consent and Communication on March 1, 2021
Part of our Sex Ed Series
Communication is the basic foundation on which healthy sexual relationships are built upon. So what does communication and consent look like?
What is Consent?
Consent in a sexual relationship means actively agreeing to be
sexual (whatever that means to you) with someone, and it goes both
ways. It is an agreement that is willfully given without any external
pressure or factors, and should be communicated freely, clearly and
coherently. An absence of a ‘no’ is not a ‘yes’. It’s important to
note that consent is not just found in sexual relationships, either.
Getting consent can happen
in lots of areas of your life, like not sharing other people’s
personal information without their permission, not touching people
without asking, and not stepping over people’s boundaries.
Importance of Consent in Sexual Relationships
According to the CDC,
“any type of sexual activity without consent is sexual assault/rape,
and is punishable by law”. A sexual activity is called sexual violence
when consent is not obtained/freely given. According to the
surveillance data by the CDC, more than 1 in 3 women and 1 in
4 men have experienced sexual violence involving physical
contact during their lifetime
For a sexual activity to be called as consensual, all parties must agree to sex willingly, every single time. If you want to get sexual with someone, it is important for you to know if the other person wants that too. Consent helps to set your personal boundaries and respecting those of your partner(s), and making sure that everyone is on the same page for any sexual activities that may occur. Consent is an ongoing process – you might agree to sex or trying something new earlier on and then change your mind – everyone has the right to do this.
The American Sexual Health Association describes that consent does not always have to be verbal, but discussing boundaries, expectations, and consent between participants at each sexual encounter is the best way to avoid confusion and respect boundaries.
Age and Consent
The minimum age at which a person can give consent for sexual
activity legally is known as the age of consent. According to the
Michigan State law, the legal age at which a person can consent to
sexual activity is 16 years of age. It’s important to
know the legal age to consent, because the consensual
age and laws vary in different parts of the United States and
different countries. Having sex with someone who is underage (younger
than the legal age) is punishable by law.
Planned Parenthood uses FRIES to explain CONSENT!
- Freely given - Giving or getting sexual consent should be a choice which is made without pressure, manipulation, and influence (drugs, alcohol, person). Asking for consent over and over until they give the answer you want is not considered as freely given.
- Reversible - Anyone can take back their given consent at any time.
- Informed - In order for someone to consent to sex, each participant must be informed and say yes to each sexual act that is performed. Sharing your STD status with your partner(s) is also a part of informed consent.
- Enthusiastic - Consent is given not only because a person wants to participate in the sexual activity, but is also excited to participate.
- Specific - Saying yes to a particular sexual activity gives you the consent for only that specific sexual act. Indulging in any other sexual activity will require consent again. For example, consent for kissing is not consent for sex.
Check out the GVSU Center for Women and Gender Equity’s FRIES video for more!
Sexual Coercion
According to the Office of Women’s Health, sexual coercion “is an
unwanted sexual activity that occurs when someone is pressured,
threatened, tricked or forced in a non-physical way to participate in
a sexual-activity.” It can be verbal or/and emotional in the form of a
statement that makes one feel pressured, guilty, shameful, or forced
through subtle actions.
Examples of Sexual Coercion include:
- “If you really loved me, you’d do it.”
- “Come on; it’s my birthday.
- “Everyone thinks we already have, so you might as well.”
- “Here, have another drink. It will loosen you up.”
- “You know I have a lot of connections.”
Check out the federal Office of Women's Health's Sexual Coercion page to learn more about it.
Communication and Sex
Communication
is the key to many problems, and so it is for a healthy,
consensual, and pleasurable sex. Communication is the basic foundation
to having a good sexual experience for yourself and your partner(s).
It’s important to not only communicate with your partner(s) about your
sexual needs, but also about your limitations.
Moreover, if you or a partner is reluctant about intensifying sexual encounters, then one should have a conversation and communicate about your comfort levels before advancing. It is important to remember the significance of checking in with your partner(s) during sexual experiences to make sure they are still okay with everything.
Here are some ways you can ask for consent:
- “Is doing ____ okay?
- “Does this feel okay?”
- “Is it okay if I do ___?”
Embrace Your Awkwards
Giving consent and getting consent may feel a bit awkward for
some people, but even then it is important to communicate clearly in
order to have healthy and consensual sexual relationships, and hence
we say: embrace your awkwards!
Some of the examples of awkward sexual conversations are as follows,
- Want to try something new in bed? Try: Hey, I have been thinking, there’s this new thing I want to try. Do you want me to explain more? Would you be interested in trying something new? I can show you what I mean if you want. If you don’t want to that’s ok, too. Is there anything you want to try?
- Want your partner(s) to get STI tested? Try making it an experience for both of you instead of just asking your partner to do it: Hey, I have heard that many STIs don’t have any symptoms and that 1 in 2 sexually active young people get an STI before the age of 25. I was thinking that maybe we could get an STI test together.
- Finding sexual activity uncomfortable and want to try lube? Try: I love what we’re doing but I think that lube might make it even better. Would you mind if we use lubrication? I have some here.
Consent and conversations may be awkward and uncomfortable to some, but ultimately, sex should be a positive and pleasurable experience for everyone and communication can help make that happen!
By: Sonal Subhash Mandale, WIT Peer Educator
Categories:
Sexual Health
Posted
on
Permanent link for Consent and Communication on March 1, 2021.
Permanent link for How Poor Sleep Can Mess You Up on February 25, 2021
I never realized how important sleep was until I started getting enough of it. A good sleep schedule can quite literally change your life! My freshman year at GVSU was rough; as a light sleeper the dorms were like my personal hell. Most nights I would only get a few hours of restless shut-eye; during the day I found myself falling asleep at inopportune moments and feeling dazed the rest of the time.
A poor sleep schedule can have very real, negative effects on people. Physically you are at risk of a weakened immunity, weight gain, and heart related problems such as high blood pressure and stroke. Maybe not so obvious, poor sleep is strongly linked to many mental disorders- it can impair your abilities to make decisions, cope with stress or change, and control emotions. These effects wreaked havoc on my life- and I didn’t even realize it was happening for so long!
Some of the biggest negative impacts of poor sleep affect your memory and ability to learn. Kind of important being students and all wouldn't you say? Did you know that basically the whole reason we ever remember anything is because we sleep? While sleeping, your brain is preparing for the next day by sorting and consolidating information into your long term memory. Sleep is absolutely necessary in order to learn and remember information!
Ok, So What Should I Do?
First step is to get enough sleep. The average college
student gets about 6-6.9 hours of sleep each night. For any
functioning adult, a bare minimum of 7 hours is needed and, unless you
are part of the 1% of our population that has an exceedingly rare
genetic mutation, this includes you! Some people need 9 (or
more!) hours.
Secondly, you’ll want to maintain a fairly regular sleep schedule. This means you should try to go to bed and wake up around the same time everyday. An irregular sleep schedule can be just as bad as not enough sleep since it messes with your circadian rhythm. Your circadian rhythm is like an internal biological clock that lets your body know when it should feel sleepy or awake. Do you ever wake up and just feel exhausted all day? You are probably suffering from irregular sleep.
Tips & Tricks to a Good Night’s Rest
How can you change your habits in order to get better sleep?
- Consider setting alarms on your phone to start establishing a sleep schedule. This means a wake-up alarm and a bedtime notification. Apple products have this function built into the clock app.
- Try to relax before bed. Don’t do any crazy activities and then try to fall asleep! Read a book or try a nighttime meditation
- Make your space comfortable. A cool, dark, quiet space is best for sleep. I use a sleep mask and, when I was living in the dorms, sound-cancelling headphones (my savior). Now I turn on a box fan or use the Relax Melodies app for some white noise.
- If you have trouble falling or staying asleep consider a melatonin supplement; something to talk to your doctor about.
- Speaking of doctors; don’t be afraid to approach your doctor if you are having an issue with sleep. Many suffer from sleep disorders such as insomnia or sleep apnea. (Learn more about the many types of sleep disorders at the Sleep Foundation’s website).
- Caffeine might get you going in the morning, but it should be stopped 4-6 hours before bedtime in order to avoid the adverse effects caffeine has on sleep.
Better Sleep = Better You
As mentioned, better sleep means better physical health, less
sickness and stress, better memory storing, and improved coping skills.
Studies
have also found that better sleep is associated with better academic
performance in college students- so by getting enough sleep and
maintaining a regular sleep routine you can be healthier, feel more
motivated, and do better in your classes! Happy sleeping!
By: Stella Sterling, WIT Peer Educator
Categories:
Sleep
Posted
on
Permanent link for How Poor Sleep Can Mess You Up on February 25, 2021.
Permanent link for Pain During Sex? on February 22, 2021
Part of our Sex Ed Series
Dyspareunia: Painful Intercourse
Have you ever experienced pain while having sex? Experiencing
cramping or pain during arousal, sex or orgasm is not uncommon,
especially for folks with vulvas. About 75% of women have painful
intercourse at some point in their lives, according to the American
College of Obstetricians and Gynecologists. The vulva and vagina are
part of the binary female, or XX-chromosome anatomy. The penis is part
of the binary male, or XY-chromosome anatomy. It is important to keep
in mind that people can identify differently than their physical
genitalia and a
person’s body may not necessarily match their gender identity.
Having painful intercourse is called dyspareunia, and it is much more common than you might think. Although the amount of research on the topic might lead one to believe otherwise, experiencing discomfort or pain can be quite common during sexual activities and is often very easily identified and resolved.
Pain for vulva owners
For vulva owners pain with sex can be experienced in the pelvic
floor, which is the group of muscles surrounding and cupping the
bladder, uterus, bowels, and rectum. These muscles are located in the
pelvis and run from the tailbone to the pubic bone, as well as
stretching from side to side of the hips. They play a large role in
sexual function and sensation, as one of the main jobs of these
muscles is to control abdominal pressure when the vagina and pelvis
are straining downwards, a common occurrence during sex and
masturbation. During orgasm or heightened arousal, the pelvic floor
muscles contract. Pain or cramping can be caused due to these muscles
cramping, similar to their reaction during the menstrual cycle. Tense
muscles can lead to pain regardless of the size or location of those
muscles. If you tighten or strain a group of muscles for an extended
period of time, there is always a chance for those muscles to react
(Pelvic Pain).
Other causes of dyspareunia include vaginal dryness, a yeast infection or UTI (urinary tract infection), STIs, and IBS (irritable bowel syndrome). Vaginal dryness can stem from stress, fear, or a naturally lower level of produced vagainal fluids. To combat this, remember to use plenty of lubricant and communicate with yourself and your partner(s) before engaging in sex. Yeast infections and UTIs can be common in vulva owners as they result from hormonal imbalances, lack of sleep, stress, and buildup of bacteria. These can be quickly taken care of with antibiotics or over-the-counter medicine. IBS or irritable bowel syndrome is a digestive/intestinal condition whose cause is unknown and whose treatments range from diets to home remedies to various medications. However in relation to pain with sexual activities, the act of penetrative sex can jostle the intestines within the pelvis and cause irritation or discomfort.
STIs can also be the source of pain or irritation during sex as they can cause lower abdominal pain, burning sensations, pain or bleeding during penetration, itching, and genital sores or warts. However the most common symptom of an STI is no symptom, which is why regular testing is important. To protect yourself and your partner(s) from STIs, use barrier methods like external or internal condoms, or dental dams.
Pain for penis owners
There are many different reasons why someone with a penis may
experience pain or discomfort during sexual activities (Penis
Pain?). The most common reasons include excessive friction,
prostatitis, an STI, or a UTI (urinary tract infection). Excessive
friction is usually caused by particularly rough sex and/or sex
without enough lubrication, as this can cause chafing. This usually
makes the penis feel sore afterwards, and can also cause
discoloration. Prostatitis is the inflammation of the prostate, which
can cause pain in the penis particularly after ejaculation. This can
be caused by bacterial infection, pelvic nerve damage, or a previous
UTI and is usually checked by a prostate exam. An uncomfortable or
painful sexual experience could also indicate a possible STI, so it is
always best to
get yourself regularly checked for STIs if you are sexually
active. Finally, UTIs could also be the the cause for pain during sex.
UTIs occur when bacteria from the digestive system infects the urinary
tract, which in penis owners is the same tract that semen flows
through during ejaculation. UTIs can also cause irritation or
inflammation of the penis, so pain during sexual activities can also
be an indicator of a separate urinary problem.
It should be noted that causes of pain for penis owners tend to be less chronic than causes of pain for vulva owners. However this doesn’t mean that penis owners should worry, or care, less about their bodies, or that if they experience pain during sex they should assume it’s less of a problem and it it will go away on its own. Pain is the body’s way of telling you that something is wrong, and it is your responsibility to listen to your body’s signals and take care of it.
Diagnosis and Treatment
If the pain you experience is ongoing and a frequent occurrence
during sex or masturbation, most healthcare professionals recommend
making an appointment with a doctor or gynecologist (for vulva
owners). Otherwise, a one-time event of pain or discomfort is said to
not be indicative of any larger problem and is most likely related
more to circumstantial factors. If you do make an appointment with
your doctor and they recommend treatment, treatments often include:
pelvic floor therapy, kegels exercises, and medication for vulva
owners, and antibiotics, topical medication, or temporary abstinence
for penis owners. Working with a sex therapist is sometimes utilized
for people whose pain is thought to be psychosomatic. Internalized
shame can often lead to people experiencing dyspareunia due to being
raised in a sex-negative household or societal pressures and stigma
around masturbation, premarital sex, or sexual orientation (Recovering
From Sexual Shame).
Don’t Be Afraid
This is not to say that you should be afraid of engaging in sex
or masturbation if you want to do so. Every person’s body is different
and some people may never experience pain or discomfort with sex or
arousal. However, for those that do, there are lots of ways to lessen
and overcome that pain. For those with vulvas, the pelvic floor
muscles can be strengthened through exercises known as kegels, where
one learns how to locate and then relax specific muscles in their
pelvis. For people with penises, ensure that generous lubrication is
being used and the penis is not being thrusted or bent at
uncomfortable angles or speeds. Alternatively, an STI test and
gynecological or prostate exam may be conducted to rule out any
diseases, bacteria or infection.
While experiencing pain during sex can cause a person to become nervous and fearful of sex and masturbation, know that it is nothing to be embarrassed or ashamed about and that for most people it is not a lifelong concern or barrier (Demystifying Painful Intercourse). However, we still need to be mindful of others’ mental health and understand how deeply an inability to be intimate with yourself or others can relate to a person’s sense of self. It can lead a person to believe that they are not normal, possibly causing sadness, grief, distress, and shame. Be mindful of those around you and remember that everybody has different boundaries, abilities, and struggles.
By: Beck Lukins, WIT Peer Educator
Categories:
Sexual Health
Posted
on
Permanent link for Pain During Sex? on February 22, 2021.